Threat Responses
Current situation
Last week Sam’s cancer journey reached a higher level of intensity. This has been a hard journey and now it is downright scary. Threats to Sam’s life are incredibly intense. First, there is the immediate threat-to-life as the cancer has caused significant damage to Sam’s vascular system and now threatens the heart itself. Second, despite the valiant effort of our medical team and Sam’s incredible courage to both understand and take on the treatments, the cancer itself continues to grow (see previous post). Medically speaking our options are limited – we need a miracle.
Despite the intensity of the current medical situation in many ways Sam appears to be healthier than he has been since before this disease began.
Medical response and plans
Maintaining blood-flow
The cancer directly or indirectly has blocked/occluded some of Sam’s major blood vessels1. As a result, blood from his head and upper body is being re-routed through an extensive network of small collateral vessels that Sam’s body has developed in compensation.
This past week we met with the intervention radiology surgical team. They have made plans to try to keep Sam’s remaining blood-flow pathways open.
On Thursday August 15 Sam is scheduled to have surgery during which stents will be inserted to maintain existing blood-flow to his heart. One will be placed in a small collateral vein that is returning the bulk of Sam’s upper body blood volume. A second stent will be used to keep the Superior vena cava open.
Additional scare – ER visit
Given everything that was revealed in the last scan our vigilance has been increased (can it go any higher?). On Sunday evening Sam started to have new/novel pains in his chest – at his heart - and strange pulsing sensations in his neck. So we went into the ER.By the time we arrived and settled in, Sam’s vitals were great. As nothing requiring immediate intervention could be determined, and given that we had a visit planned with Sam’s medical team the next day, we returned to RMH.
Disease control
It is unknown if this cancer can be controlled but that does not mean we will stop trying. In response to the latest scans we will push on and push harder. Greater risks must be taken. Treatments must be accelerated.
The original plan was to attempt an increase in Sam’s Nivolumab by doubling the dose. Given the latest results we have chosen to push harder. Wednesday the dose was quadrupled in an effort to find an effective dose – though it will take a few weeks to know if it is having the desired effect.
In addition, Sam is back on high-dose steroids (prednisone). One of the primary reasons to use this drug is to quickly reduce inflammation in the body. Sam has also used it in the past to protect his liver which the Nivolumab can harm. Within 24 hours of starting the drug it was possible to visibly see positive impacts.
Friends and family
This past week it was amazing to have the in-person support of some friends and family from Prince George. We had great visits and times that simply felt normal.
Joel, Joanna, and Chase were here for Friday evening and Saturday. We shared meals, went to a movie (Inside Out 2 – it is great!), made an ice cream run, Chase and Sam threw a football around, and played some video games together.
Sunday and Monday my parents came to spend time with us. The effects of the Nivolumab started to set in on Sunday – causing fatigue. However, that did not stop us from spending time and sharing meals together. Sam loved having his grandparents here. Sam seems to be loving his ice cream these days (could be the prednisone) so to wrap up our time together we celebrated with an ice cream cake that Sam requested from DQ.

Victories and concerns
The cancer has grown and the impacts of the disease are threatening Sam’s vascular system and thereby his life.
Sam will have surgery, planned for August 15, to install stents to protect the blood-flow returning to his heart. This is an unusual surgery as Sam’s vasculature is abnormal - the most trusted doctors with the most expertise to deal with this risky procedure have been asked to perform it.
Sam is on higher levels of Nivolumab. Side effects of this medication include fatigue and agitation of the liver. In the past we were not able to use this drug for numerous weeks due to liver inflammation. Current support medications are being used to reduce negative side effects.
To date, the medicines and interventions that have been tried have not had any significant or lasting effect at controlling this disease. We need something that will work. We need a miracle.
It was amazing to see Sam join the Ness Lake Bible Camp team (July 28 - 31) . He served, ran, talked, played – he got to be fully there! Many thanks to the NLBC team who welcomed him in.
We are thankful to the medical team here at BC Childrens’ Hospital who have explained things incredibly well and who have worked professionally and confidently. Your clear communication, compassion, and medical care give us great confidence.
We are thankful for the gift of a place to stay so close to where Sam is receiving his care. The Ronald McDonald House (RMH) has provided us a home away from home. This place is an amazing example of charity at work.
Thankful for friends who have chosen to meet regularly to pray for Sam (we are also thankful for everyone praying for Sam whereever you are). If you would like to join them talk with Beth H., Krista C., or contact the Westwood Church office.
Thankful for such supportive family and friends caring for us all through this journey.
We long for the day when Sam is free of this disease.
Footnotes
- ↩︎
The left and right bracheocephalic veins are fully occluded. The right was occluded when we first arrived due to blood clotting associated with the disease. As of last week’s scans the left is also now fully occluded. Sam’s body has adapted rerouting blood through collateral vessels. One of these small vessels returns blood directly into the Superior vena cava (SVC). Blood return through other collaterals is collected by the Azygos vein.
An additional issue is that the SVC is also partially occluded (~50%).
Surgery this week will insert stents to ensure that a) the one collateral returning blood directly to the SVC remains open, and b) That the SVC itself remains open.
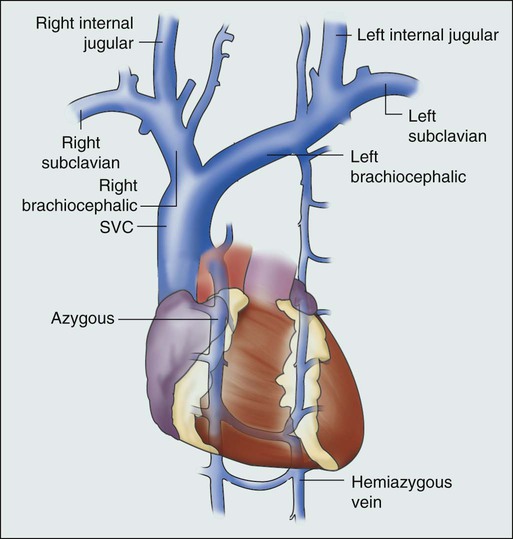
The heart and major veins returing deoxygenated blood from the upper body to the heart.